If you’ve ever searched online because you noticed unusual fatigue, sugar cravings, weight changes, or symptoms that made you worried about diabetes — you’re not alone. Understanding the difference between Type 1 and Type 2 diabetes symptoms and treatment is one of the most important steps in taking control of your health.
Both conditions involve high blood sugar, but the way they develop, how the symptoms show up, and how they are treated are very different. One type happens because the body can’t produce insulin, and the other develops because the body cannot use insulin properly. When you understand why diabetes happens, you also begin to understand what can be prevented and what cannot. So now, let’s move deeper into the real cause of both conditions — gently, one step at a time.
What Is the Difference Between Type 1 and Type 2 Diabetes Symptoms?
If you’ve ever wondered why some people need insulin from day one while others manage diabetes with lifestyle changes, diet, or tablets — the answer lies in understanding the difference between Type 1 and Type 2 diabetes symptoms and treatment.
At first glance, both conditions sound similar because they involve high blood sugar. But when you look deeper, their causes, symptoms, treatment approach, and long-term care are very different. Think of it like this:
Both conditions speak the same language — but they come from different worlds.
Let’s break it down slowly and simply.
Quick Overview of Type 1 Diabetes
Type 1 diabetes is an autoimmune condition. That means the body isn’t doing something wrong — it’s misunderstanding something.
Imagine your immune system as your body’s security guard. Its job is to protect you. But in Type 1 diabetes, this guard becomes confused and starts attacking the very cells in the pancreas that make insulin. Over time, this destruction becomes permanent.
So, people with Type 1 diabetes don’t have insulin — or have very little. And without insulin, glucose can’t enter the cells. Instead, it builds up in the bloodstream. That’s why insulin therapy isn’t optional for Type 1 diabetes — it’s necessary. Type 1 usually starts in childhood or young adulthood, but it can appear at any age. It develops quickly — sometimes within weeks — and symptoms can be intense.
✔ To understand Type 1 deeply, read this: Type 1 Diabetes Symptoms Guide
Quick Overview of Type 2 Diabetes
Now, Type 2 diabetes is different — here, the body still produces insulin, sometimes even more than normal. But the cells stop responding to it properly. This condition is called insulin resistance. Think of it like someone knocking on a door. Earlier, the door opened easily. But slowly, the lock becomes rusty and harder to open. The body keeps producing more insulin to push that door — but eventually, it becomes too difficult. Type 2 diabetes develops gradually — sometimes over years — which is why early warning signs are easy to miss. Many people discover it accidentally during a routine check-up. The good news? Type 2 diabetes can often be managed or improved with nutrition, weight management, exercise, medications, and lifestyle change.
✔ To understand Type 2 deeply, read this: Early Signs of Type 2 Diabetes
Key Differences (Fast Comparison — Explained Simply)
Instead of a chart, let’s understand this in a relatable way:
| Topic | Type 1 | Type 2 |
|---|---|---|
| Cause | Autoimmune attack destroys insulin-producing cells | Body still makes insulin, but cells stop responding |
| Age group | More common in children/young adults | More common in adults, but rising in teens |
| Treatment | Insulin required for life | Lifestyle changes + medication, insulin only if needed |
| Progression | Fast | Slow and gradual |
| Prevention | Not preventable | Often preventable and reversible in early stages |
So the major difference between Type 1 and Type 2 diabetes symptoms and treatment is that Type 1 requires insulin because the body no longer makes it, while Type 2 focuses more on improving insulin sensitivity and lifestyle changes.
Compare Type 1 vs Type 2 Diabetes Causes and Prevention
Understanding the root cause of diabetes helps you understand the disease better, reduces fear, and gives clarity about what you can control — and what you cannot. Even though both Type 1 and Type 2 diabetes result in elevated blood sugar levels, their causes are very different. One develops suddenly and unpredictably, while the other builds slowly over years.

Causes of Type 1 Diabetes
The truth is — Type 1 diabetes is not something a person can control or avoid. It happens because the immune system mistakenly destroys the insulin-producing cells in the pancreas. It’s like the body is confused and starts attacking itself, believing those insulin-producing cells are harmful.
Researchers believe several factors may trigger this condition:
- Genetics and family history: If someone has a close family member with Type 1 diabetes, the risk is slightly higher — but even then, not guaranteed. Many people with no genetic history also develop it.
- Autoimmune response: The immune system, which should ideally protect the body, mistakenly destroys the beta cells that produce insulin.
- Possible viral triggers: Some studies suggest that certain viral infections may trigger this immune reaction — but this isn’t proven for everyone.
- Environmental factors: Situational triggers may contribute, but there is no single identified cause.
Type 1 diabetes is NOT caused by eating sugar, having an unhealthy lifestyle, or making a mistake. Parents of children diagnosed with Type 1 diabetes sometimes blame themselves — but please remember: Nothing you did or didn’t do caused this.
Causes of Type 2 Diabetes
Type 2 diabetes develops slowly — sometimes over many years — and often goes unnoticed during early stages. Unlike Type 1, the pancreas still makes insulin, but the cells stop responding to it properly. This condition is called insulin resistance. Several contributing factors can lead to Type 2 diabetes:
- Insulin resistance building over time: The body continues producing insulin, but cells no longer respond effectively, causing blood sugar levels to rise.
- Genetic influence: If diabetes runs in the family, the risk increases — but lifestyle still plays a huge role in how or when it develops.
- Weight management and belly fat: Fat stored around the abdomen interferes with how the body uses insulin, increasing insulin resistance.
- Sedentary lifestyle: Lack of regular movement affects metabolism and blood sugar regulation.
- Diet high in processed foods and sugar: Frequent intake of sugary drinks, refined grains, and junk food increases the risk.
- Stress and poor sleep: Chronic stress and lack of sleep can disrupt hormones that regulate insulin and appetite.
Type 2 diabetes doesn’t appear suddenly — it’s the result of many small habits and changes that slowly build up over time.
Can Type 1 Diabetes Be Prevented?
As of today Type 1 diabetes cannot be prevented. Because it is autoimmune and genetic in nature, lifestyle changes or diet adjustments do not stop it from happening. Research is ongoing, especially in immune-modulating treatments, but currently there is no proven prevention.
Prevention Tips for Type 2 Diabetes
The empowering part is — Type 2 diabetes can often be prevented, delayed, or even reversed in early stages through small, consistent lifestyle habits. Here’s what truly helps:
- Move your body regularly: Even 20–30 minutes of walking a day improves insulin sensitivity, reduces belly fat, and stabilizes blood sugar.
- Choose balanced and whole foods: Eating fiber-rich fruits, vegetables, whole grains, and protein helps the body use insulin efficiently.
- Limit processed sugars and refined carbs: Reducing sugary drinks, white bread, and packaged snacks prevents spikes in blood sugar.
- Maintain a healthy body weight: Even a small weight reduction (5–7%) significantly lowers the risk.
Prioritize stress reduction and sleep: Good sleep and calming habits like deep breathing, yoga, or journaling help control blood glucose response.
Which Is More Common: Type 2 Diabetes or Type 1 Diabetes in Adults?
When we talk about the difference between Type 1 and Type 2 diabetes, one of the biggest practical differences is how common each type is — especially in adults. While both are serious conditions, they don’t occur in the same pattern or at the same frequency.
Diabetes Statistics Worldwide
Globally, diabetes is increasing at a fast pace especially because of changing lifestyles, urbanization, and lack of physical activity. But here’s the key fact:
- About 90–95% of all diabetes cases are Type 2, while
- Only about 5–10% are Type 1
So yes — Type 2 diabetes is much more common, especially among adults. Type 1 diabetes is comparatively rare and usually appears earlier in life, although adults can develop it too.

Why Type 2 Is More Common in Adults
There are several reasons why Type 2 diabetes is more common in adults, and most of them are linked to lifestyle, environment, and long-term habits.
- Many adults experience:
- Increased stress
- Irregular meal patterns
- Long sitting hours
- Processed or fast-food–based diets
- Weight gain, especially belly fat
- Less physical movement
Over time, these factors reduce the body’s sensitivity to insulin, a process known as insulin resistance. Even if someone genetically has a risk, lifestyle accelerates the condition. Type 1 diabetes, on the other hand, does not depend on lifestyle — it’s autoimmune and unpredictable.
Rising Trends in Children and Teens
Even though traditionally:
- Type 1 was associated with children, and
- Type 2 was considered an adult condition
This pattern is changing.
Today, children and teenagers are increasingly being diagnosed with Type 2 diabetes — mainly due to:
- Reduced outdoor activity
- Increased screen time
- High consumption of sugary drinks and processed snacks
- Obesity and early insulin resistance
So while Type 1 remains more common in kids, Type 2 cases in younger age groups are dramatically rising worldwide — which is a concern.
Early Symptoms Comparison
Since we’re discussing the difference between Type 1 and Type 2 diabetes symptoms, understanding the symptoms helps you recognize the condition early. Even though both involve high blood sugar, the way symptoms appear is different.
Symptoms of Type 1 Diabetes
Type 1 diabetes usually develops quickly — sometimes within weeks or even days.
Symptoms can be intense and sudden because the body stops producing insulin almost completely.
People may notice:
- Rapid and unexplained weight loss
- Extreme thirst and hunger
- Frequent urination (especially at night)
- Fatigue and weakness
- Blurred vision
- Nausea or vomiting (in severe cases)
Because of the fast onset, Type 1 often becomes noticeable earlier.
Symptoms of Type 2 Diabetes
Type 2 diabetes develops slowly — sometimes over years — and many people don’t notice symptoms in the beginning.
Early signs may include:
- Increased thirst and urination
- Fatigue and low energy
- Slow-healing wounds
- Darkened skin patches (acanthosis nigricans)
- Frequent infections (skin, gums, urinary tract)
- Tingling or numbness in hands or feet
Type 2 diabetes is often diagnosed during routine checkups, because symptoms can be subtle.
Symptoms That Overlap in Both Forms
Since blood sugar rises in both conditions, some symptoms are common:
- Excessive thirst
- Frequent urination
- Fatigue
- Increased hunger
- Blurred vision
So even though the causes and speed of onset differ, the body signals high glucose in similar ways.
How Treatment Differs for Type 1 vs Type 2 Diabetes
Now, let’s talk about treatment — because this is one of the most important areas where the difference between Type 1 vs Type 2 diabetes becomes very clear.
Treatment for Type 1 Diabetes (Insulin-Based)
Since the body produces little or no insulin, treatment relies on:
- Daily insulin injections
- Insulin pumps
- Blood glucose monitoring
- Carbohydrate counting
There’s no cure yet, and lifestyle cannot replace insulin — but a balanced diet, regular movement, and emotional support make management smoother.
Treatment for Type 2 Diabetes Symptoms (Lifestyle + Medication)
For Type 2 diabetes, treatment is flexible and depends on how early the condition is caught.
It may include:
- Lifestyle changes (diet + movement)
- Weight management
- Oral medications like Metformin
- Insulin (only if necessary, usually in later stages)
In the early stage, some people can reverse or control diabetes simply by improving their lifestyle.
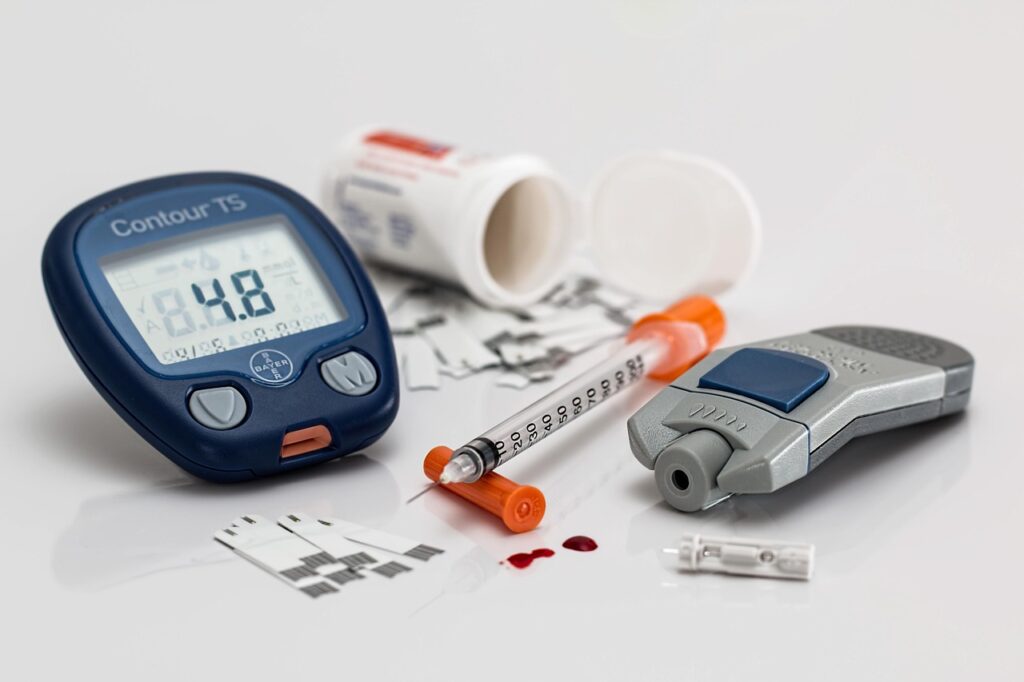
Monitoring Tools (CGM, Glucometer, A1C Testing)
Whether Type 1 vs Type 2 — monitoring is essential.
Common tools include:
- Glucometers — daily finger-prick glucose checks
- CGM (Continuous Glucose Monitors) real-time automatic tracking
- A1C tests — shows 3-month blood sugar average
Type 1 vs Type 2 Diabetes: Diet and Lifestyle Comparison Guide
Understanding the difference between Type 1 and Type 2 diabetes symptoms and treatment is helpful, but diet and lifestyle also play a huge role in managing both conditions. Even though both involve high blood sugar, their dietary focus and goals are slightly different.
Diet Recommendations for Type 1 Diabetes Symptoms
In Type 1 diabetes symptoms, the main goal is balancing food and insulin. Since the body cannot produce insulin, people must pay attention to how many carbohydrates they eat because carbs directly affect blood sugar levels. The diet does not have to be restrictive, but it must be planned. Whole foods, fiber-rich meals, lean proteins, healthy fats, and slow-digesting carbohydrates help keep sugar levels more stable. Instead of avoiding food, learning portion control and carb counting becomes important.
Diet Recommendations for Type 2 Diabetes Symptoms
For Type 2 diabetes symptoms, diet focuses more on reducing insulin resistance and supporting weight management. Eating balanced meals with vegetables, whole grains, legumes, proteins, nuts, seeds, and fruits helps maintain steady glucose. Many people benefit from reducing portion size, limiting sugary snacks, and choosing foods with lower glycemic index. The hopeful part is that small changes — even replacing one processed meal with a homemade one — can make a noticeable difference over time.
Physical Activity and Weight Management
Movement is important in both conditions, but the purpose is different. In Type 1 diabetes, physical activity can help improve insulin absorption and maintain stable glucose — but levels must be monitored because exercise can lower sugar quickly.
In Type 2 diabetes symptoms, regular exercise — even a 20–30 minute walk — can improve insulin sensitivity, reduce weight, and stabilize energy. Consistency matters more than intensity.
Foods to Avoid in Both Conditions
Even though everyone’s body responds differently, some foods tend to cause blood sugar spikes in both Type 1 and Type 2 diabetes. These include sugary drinks, packaged snacks, fast food, refined white flour products, and heavily processed items. Avoiding them does not mean giving up taste — instead, it means shifting toward healthier alternatives that support long-term well-being.
Complications If Not Managed Properly
Managing blood sugar isn’t just about controlling numbers — it’s about protecting long-term health. When diabetes (whether Type 1 or Type 2) is not managed, complications can slowly develop.
✔ For full diabetes overview, read: Diabetes Explained
Short-Term Risks (DKA vs Hyperglycemia)
In Type 1 diabetes, the most serious short-term risk is Diabetic Ketoacidosis (DKA) , a dangerous condition caused by lack of insulin. In Type 2 diabetes symptoms, the common short-term issue is hyperglycemia, where blood sugar stays high for long periods and causes weakness, dehydration, and fatigue.
Long-Term Damage (Heart, Eyes, Kidney, Nerves)
If diabetes remains uncontrolled for years, it can affect several organs regardless of whether it is Type 1 or Type 2. High blood sugar can harm the heart, kidneys, nerves, and vision. Many people with long-standing uncontrolled diabetes may develop neuropathy, kidney disease, or vision changes. The good news? Early management and consistent monitoring greatly reduce these risks.
Type 1 vs Type 2 Diabetes Across Age Groups
The difference between Type 1 and Type 2 diabetes symptoms can vary by age. Children, adults, and seniors may experience diabetes differently based on lifestyle, health status, and metabolism.
Children & Teens
Type 1 diabetes is more common in younger age groups and often begins suddenly. Kids may experience rapid weight loss, bedwetting due to frequent urination, fatigue, or extreme thirst. In recent years, Type 2 diabetes symptoms has also been rising in children — mostly due to inactivity and poor diet patterns.
Adults
Type 2 diabetes symptoms is most common in adults and can develop quietly over many years. Adults may mistake early symptoms for stress or tiredness. Type 1 can also occur in adults, although it is less common and usually appears more suddenly.
Seniors
In older adults, diabetes may show up with subtle signs such as fatigue, confusion, weakness, or frequent infections. Seniors with Type 2 diabetes may need a modified diet and adjusted medications depending on mobility, appetite, and other health conditions.
FAQs
1. What is the main difference between Type 1 and Type 2 diabetes symptoms?
The main difference between Type 1 and Type 2 diabetes symptoms and treatment is that Type 1 is autoimmune and requires insulin, while Type 2 is linked to insulin resistance and may be managed with lifestyle changes, medication, or insulin.
2. Which type of diabetes is more common in adults?
Type 2 diabetes is far more common in adults compared to Type 1.
3. Can Type 2 diabetes turn into Type 1?
No — Type 2 diabetes cannot convert into Type 1 because both have different causes.
4. Can Type 1 diabetes be prevented?
No, Type 1 diabetes cannot currently be prevented because it’s autoimmune.
5. Can Type 2 diabetes symptoms be prevented?
Yes — healthy eating, movement, weight management, and sleep can lower risk.
6. How is treatment different for Type 1 vs Type 2 diabetes symptoms?
Type 1 requires insulin from the start. Type 2 symptomsmay use lifestyle changes, oral medication, or insulin depending on severity.
7. What symptoms are common in both types?
Increased thirst, excessive urination, fatigue, blurred vision, and unintended weight changes.
8. Is Type 2 diabetes reversible?
In early stages, some people can reverse Type 2 through diet, exercise, and lifestyle changes.
9. Do children get Type 2 diabetes?
Yes — although rare earlier, Type 2 cases in children and teens are increasing worldwide.
10. Which type of diabetes is easier to manage?
Type 2 diabetes may be easier for some people to manage because lifestyle habits have a strong impact, unlike Type 1.
Summary — Difference Between Type 1 and Type 2 Diabetes Symptoms and Treatment
Understanding the difference between Type 1 and Type 2 diabetes symptoms and treatment is essential because both conditions affect the body differently, and their management pathways are not the same. Type 1 diabetes is autoimmune and usually develops suddenly, requiring lifelong insulin therapy. Type 2 diabetes often develops slowly and is strongly linked to lifestyle, weight, genetics, and insulin resistance.
When we compare Type 1 vs Type 2 diabetes causes and prevention, Type 1 cannot currently be prevented, while Type 2 can often be delayed, reduced, or even reversed in early stages through healthy habits.
If you ask which is more common — Type 2 diabetes or Type 1 diabetes symptoms in adults, the answer is clear: Type 2 diabetes is significantly more common. However, cases of both forms are rising in younger age groups.
Another important point is how treatment differs for Type 1 vs Type 2 diabetes. Type 1 requires insulin from the beginning because the body produces none. Type 2 treatment may begin with physical activity, dietary modification, and medication — and some people may later require insulin if their body’s insulin response weakens over time.
To make decisions easier, this Type 1 vs Type 2 diabetes: diet and lifestyle comparison guide helps explain how food choices, physical activity, weight management, and long-term habits affect blood sugar levels differently in both conditions. Eating balanced whole foods, maintaining daily movement, reducing processed sugar, and monitoring glucose levels can support better control — regardless of the type.
Final Thought
You don’t need to remember everything in one day — just understanding the difference between Type 1 and Type 2 diabetes symptoms and treatment gives you power. Whether prevention, comparison, or lifestyle support, every small step forward can improve health and confidence.
✔ If you still have doubts, visit: Diabetes FAQs
Disclaimer:
The information shared here is intended solely for general awareness and educational purposes. It should not be considered a substitute for professional medical advice, diagnosis, or treatment. While this content may refer to general health guidelines from trusted organizations, it may not be suitable for your specific health needs. Please consult a licensed healthcare professional before making decisions related to medication, supplements, diet, or diabetes care.
References used for general knowledge include:
- World Health Organization (WHO)
- Centers for Disease Control and Prevention (CDC)
- American Diabetes Association (ADA)
Everyone’s health journey is unique, and results may vary. By accessing or using this information, you acknowledge that the creator or publisher is not responsible for any outcomes or decisions made based on this content.
3 thoughts on “Difference Between Type 1 and Type 2 Diabetes Symptoms (Complete Guide)”