What Are the Early Signs of Type 2 Diabetes?
Let’s make this simple and honest. Most people don’t notice the early signs of Type 2 diabetes because they start slowly. It’s not like one morning you wake up and suddenly know something is wrong — instead, your body gives small signals over time.

If lately you’ve been thinking,
- Why am I always tired?
- Why am I so thirsty?
- Why is my body behaving differently?
then understanding the early signs of Type 2 diabetes may help you make sense of what’s happening. So let’s break it down gently, clearly, and with real examples.
Frequent Urination & Constant Thirst
One of the most common early signs of Type 2 diabetes is needing to pee more often and feeling thirsty all the time, sometimes even waking up at night for water.
How it actually feels:
You drink a glass of water, then another… but your mouth still feels dry. You may think, “Maybe I didn’t sleep well,” “Maybe I ate something salty,” but deep down you know it feels unusual.
Why it happens:
When blood sugar rises, the kidneys try to remove extra glucose. To do that, they pull more water from your body, which leads to:
- More urination
- More dehydration
- More thirst
If this feels familiar, note it — it’s one of the strongest early signs of Type 2 diabetes.
What to do right now:
- Track how many times you urinate daily and at night
- Notice when thirst increases morning, after meals, or always
Constant Fatigue and Low Energy
Another big indicator among the early signs of Type 2 diabetes is unusual tiredness, the kind that doesn’t go away even after rest.
What it feels like:
You may sleep a full night, yet wake up tired. Simple tasks feel heavier. Your mind feels foggy, and afternoon energy crashes become predictable.
Why it happens:
Your body has sugar, but cells can’t use it properly because insulin isn’t working efficiently. So it’s like having food but not being able to eat it — the energy is there, but locked.
Simple helpful steps:
- Take a 10–15 minute walk after meals
- Track when fatigue shows up (before or after eating?)
This is one of the early signs of Type 2 diabetes people ignore the longest because they think it’s “normal tiredness.”
Sudden Weight Loss or Belly Weight Gain
Changes in weight without explanation are also part of the early signs of Type 2 diabetes.
How it looks:
Unintentional weight loss: Body breaks fat and muscle for energy because cells aren’t using glucose. Weight gain, especially belly fat: Due to insulin resistance, the body stores extra fat around the abdomen. If weight changes don’t match your lifestyle, don’t ignore it — it can be a hidden clue.
What you can do:
- Track weight weekly
- Notice waist measurement instead of just the scale
Blurry Vision & Slow-Healing Wounds
These are less obvious but important early signs of Type 2 diabetes.
Blurred Vision:
Sometimes your vision becomes fuzzy for a few hours — especially after meals. You may think it’s screen time or tiredness, but fluctuating glucose can temporarily change the shape of the eye lens.
Slow Healing:
Small cuts take longer to heal. Scratches, insect bites, shaving cuts — all seem to heal slowly because high glucose reduces blood flow and affects immunity. If this keeps happening, it may be one of the clearer early signs of Type 2 diabetes.
Tingling or Numbness in Hands & Feet
This symptom shows up when high sugar starts affecting nerves.
How it feels:
- Tingling
- Burning
- Pins-and-needles
- Numbness that comes and goes
It may start mild but gradually become more noticeable — especially at night. Because this happens after prolonged high sugar, it is considered one of the later early signs of Type 2 diabetes, and catching it early may prevent long-term nerve damage.
If two or more of these symptoms feel familiar, it doesn’t mean panic — it means awareness. The moment you notice the early signs of Type 2 diabetes, you give yourself a chance to take control early.
And early action = easier management + better health.
Early Signs of Type 2 Diabetes in Women vs Men
Even though the early signs of Type 2 Diabetes can look similar in both men and women, the body reacts differently based on hormones, metabolism, and lifestyle. Understanding these differences can help in catching the condition sooner — and early detection is always better than waiting for symptoms to worsen. Many people ignore mild symptoms in the beginning because they seem normal — like tiredness, mood swings, or increased thirst. But the truth is, these could be important early signs of Type 2 Diabetes that your body is trying to communicate.
Let’s break this down for both women and men clearly and simply:
Symptoms in Women
Women often experience hormonal fluctuations throughout life — puberty, pregnancy, menstruation, menopause — and these can sometimes mask or confuse the early signs of Type 2 Diabetes.

Here are the most common symptoms seen in women:
Frequent yeast infections or UTIs
High blood sugar creates the perfect environment for fungal growth and infections. If infections keep coming back, it’s a red flag.
Unexplained fatigue or mood changes
When blood sugar remains high, the cells don’t get enough energy — making you feel irritated, tired, or mentally drained.
Weight changes (especially weight gain around the belly area)
Insulin resistance often leads to abdominal fat storage, making weight loss difficult.
Irregular menstrual cycle
Hormonal balance gets affected, especially when insulin resistance increases.
Slow wound healing
Cuts, acne scars, or injuries take longer to heal due to poor blood circulation. Skin darkening around neck, underarms, or groin (Acanthosis Nigricans)
This is a very common physical warning sign and one of the most noticeable early signs of Type 2 Diabetes.
Many women ignore these symptoms thinking they’re due to stress, PCOS, hormonal imbalance, or lifestyle — but if these symptoms stay longer than 2–4 weeks, it’s important to get checked.
Symptoms in Men
Men may also experience the common early signs of Type 2 Diabetes, but some symptoms are more specific due to metabolic and hormonal differences.
Common symptoms seen in men include:
Low energy and constant tiredness
When insulin isn’t working properly, sugar stays in the blood instead of being used as energy — leading to fatigue.
Erectile dysfunction or low libido
High blood sugar affects nerves, blood flow, and testosterone levels — which may affect sexual health.
Muscle weakness or loss of muscle mass
The body starts breaking down muscle for energy if glucose isn’t being absorbed properly.
Increased hunger and cravings
Even after eating a full meal, the brain signals hunger because cells aren’t receiving glucose.
Vision problems like blurred or fluctuating eyesight
High sugar affects the eyes early on, which is another overlooked sign. Just like women, men may dismiss these symptoms as aging, stress, lack of sleep, or lifestyle — but when multiple symptoms show up together, they shouldn’t be ignored.
Type 2 Diabetes Risk Factors
Understanding risk factors is just as important as knowing the symptoms. Sometimes people don’t notice the early signs of Type 2 Diabetes because the body adapts gradually — but risk factors can warn you way before symptoms appear.
Here are the major Type 2 Diabetes risk factors:
Family History & Genetics
If your parents, siblings, or close family members have Type 2 Diabetes, your risk naturally increases. Genetics doesn’t guarantee diabetes — but it makes your body more sensitive to insulin resistance.
Obesity & Sedentary Lifestyle
Excess body weight — especially belly fat — increases Type 2 Diabetes risk factors dramatically because fat cells interfere with insulin efficiency. Long sitting hours, lack of exercise, and low muscle activity make insulin resistance even worse.
Polycystic Ovary Syndrome (PCOS)
For women, PCOS is one of the strongest risk factors. PCOS often comes with hormonal imbalance, weight gain, and insulin resistance — making women more prone to developing diabetes earlier in life. If a woman has PCOS and experiences the early signs of Type 2 Diabetes, she should take them seriously.
Age, Stress & Poor Sleep
As we age, metabolism naturally slows down — especially after age 40. But today, lifestyle stress and poor sleep are affecting even younger people. Chronic stress increases cortisol, which raises blood sugar. Lack of sleep affects appetite, insulin sensitivity, and energy levels. Irregular routine increases both Type 2 Diabetes risk factors and symptoms. Whether you’re a man or a woman, the most important thing is awareness. The early signs of Type 2 Diabetes are your body’s warning signal — and recognizing them early can prevent complications like nerve damage, kidney issues, heart disease, or vision loss. If these symptoms or risk factors sound familiar — don’t panic. Instead, see it as an opportunity to take control of your health before diabetes takes control of you.
Type 2 Diabetes Blood Sugar Chart (To Help Identify Early Signs)
Sometimes, symptoms can be confusing but numbers never lie. A blood sugar chart helps you understand whether your glucose levels fall in the normal range or point toward the early signs of Type 2 Diabetes.
Here is a simple table for clear understanding:
| Test Type | Normal Range | Prediabetes Range | Type 2 Diabetes Range |
|---|---|---|---|
| Fasting Blood Sugar (Before Eating) | 70–99 mg/dL | 100–125 mg/dL | 126 mg/dL or higher |
| Post-Meal Test (2 Hours After Eating) | Less than 140 mg/dL | 140–199 mg/dL | 200 mg/dL or higher |
| A1C (3-Month Average) | Below 5.6% | 5.7%–6.4% | 6.5% or higher |
| Random Sugar Test | Below 140 mg/dL | 140–199 mg/dL | 200 mg/dL or higher |
If your numbers stay in the prediabetes or Type 2 Diabetes range, it’s a good idea to talk with a doctor and start lifestyle changes early.
How Is Type 2 Diabetes Diagnosed?
If someone is experiencing the early signs of Type 2 Diabetes, the next step is testing. Diagnosis isn’t based on just symptoms but a combination of tests that confirm blood sugar levels over time.
A1C Test
The A1C test measures the average blood sugar levels of the last 2–3 months. It does not require fasting and is often the first test doctors use. If your A1C is 6.5% or higher, it usually indicates diabetes.
Fasting Glucose Test
This test is done after 8–12 hours of fasting (no food or drinks except water). It helps understand how your body handles blood sugar without food. A fasting level of 126 mg/dL or above indicates Type 2 Diabetes.
OGTT Test (Oral Glucose Tolerance Test)
In this test:
1. Your fasting sugar level is checked.
2. You drink a sugary liquid.
3. Blood sugar is checked again after 2 hours.
If the result is 200 mg/dL or higher, it confirms diabetes.
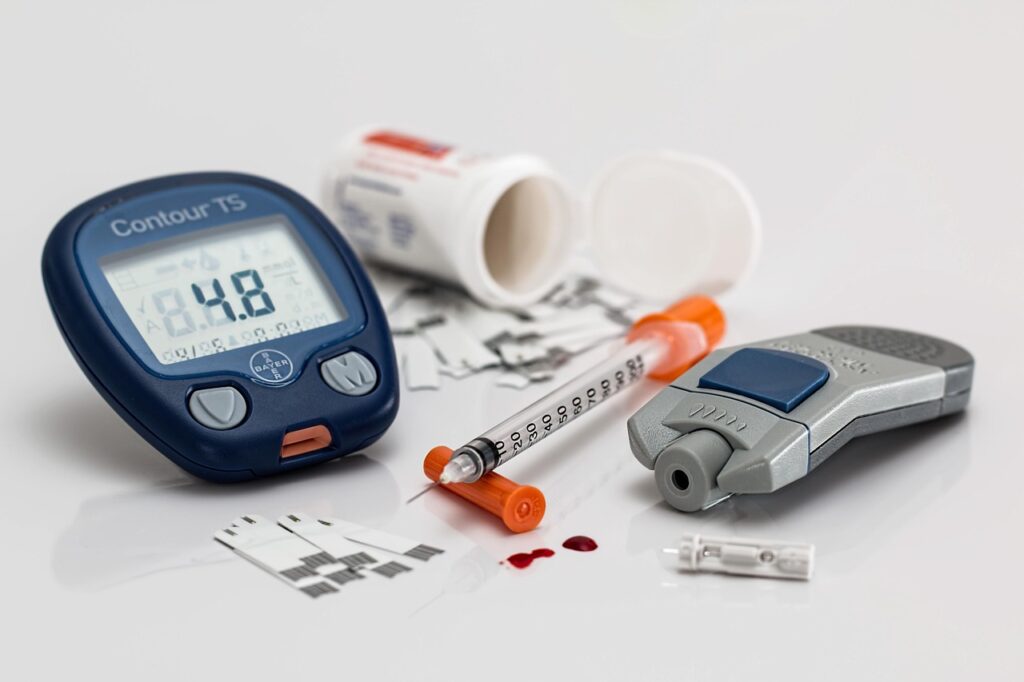
Self-Monitoring at Home
Today, with glucometers and continuous glucose monitors (CGM), many people track blood sugar at home.
Self-monitoring helps in:
- Detecting the Early Signs of Type 2 Diabetes
- Understanding food triggers
- Tracking improvement after lifestyle changes
Can Type 2 Diabetes Be Reversed Naturally?
A lot of people ask:
“Is it really possible to reverse Type 2 Diabetes naturally?” The honest answer is: Yes — for many people, reversal is possible.
But it requires lifestyle consistency, awareness, and sustainable habits.
What Science Says
Research shows that when the body becomes insulin-resistant, fat builds up in the liver and pancreas. Reducing this internal fat through lifestyle changes can help some people restore normal blood sugar levels — especially in the early stage. So, if someone recognizes the early signs of Type 2 Diabetes and takes action early, the chances of reversal are much higher.
How Reversal Works
Reversal doesn’t mean diabetes magically disappears — it means:
- Blood sugar stays in healthy range
- No medications are needed (in many cases)
- Insulin sensitivity improves
Reversal happens when:
- Diet improves
- Weight loss is achieved (especially belly fat)
- Exercise becomes consistent
- Stress & sleep are managed
- Ultra-processed food is reduced
It’s a journey not a quick fix but it is possible.
✔ For complete explanation of diabetes types and causes: Diabetes Explained (Main Guide)
Type 2 Diabetes Diet Plan
Food plays the biggest role in controlling diabetes — because what you eat directly affects blood sugar. A healthy diet can prevent symptoms from getting worse and support reversal if done correctly.

- Best Foods to Control Blood Sugar
- Here are foods that keep sugar stable and fuel the body gently:
- Vegetables (especially leafy greens)
- High-fiber fruits like berries, apples, pears
- Whole grains (oats, brown rice, quinoa)
- Beans and lentils
- Nuts and seeds
- Eggs, fish, chicken (if non-veg)
- Avocado and healthy fats
- Greek yogurt (unsweetened)
These foods help reduce insulin resistance and support weight control — which is helpful when dealing with the early signs of Type 2 Diabetes.
Foods to Avoid
Some foods cause a sharp spike in blood sugar and make symptoms worse:
- Sugary drinks (cola, juice, energy drinks)
- White bread, pasta, bakery items
- Fried and fast food
- Candies, chocolates, sweets
- Artificially flavored or processed packaged food
Reducing these makes a big difference in maintaining sugar levels.
Sample 1-Day Meal Plan
Here’s a balanced meal plan example:
| Time | Meal Suggestion |
|---|---|
| Breakfast | Oatmeal with berries + chia seeds |
| Mid-Morning Snack | A handful of almonds or an apple |
| Lunch | Brown rice or quinoa + vegetables + dal or grilled chicken |
| Evening Snack | Green tea + roasted chana |
| Dinner | Soup + salad + small portion of protein |
| Optional After-Dinner | Sugar-free herbal tea |
This pattern keeps sugar levels stable and prevents large up-and-down spikes.
Best Exercises for Type 2 Diabetes
Movement is one of the most powerful ways to support blood sugar control — especially if someone is noticing the Early Signs of Type 2 Diabetes. You don’t need a gym membership or complicated routines. Small, consistent habits make the biggest impact.
Let’s explore simple exercises that work for real life:
Walking & Daily Movement
Walking is one of the easiest and most effective ways to improve insulin sensitivity.
What it does:
- Helps reduce blood sugar spikes after meals
- Supports weight loss
- Improves heart health
- Reduces stress hormones
Try this small habit:
- Take a 10–15 minute walk after each meal.
This single routine can dramatically improve glucose levels.
Strength Training
Strength training builds muscle — and muscles act like a “glucose sponge,” absorbing sugar from the bloodstream.
Examples of beginner-friendly exercises:
- Squats
- Lunges
- Wall push-ups
- Light dumbbell or resistance band workouts
Start with 2–3 sessions per week, even if it’s just 15–20 minutes. Consistency matters more than perfection.
Yoga & Breathing Practices
Yoga helps reduce inflammation, balance hormones, and improve insulin response. Breathing practices also lower stress, which plays a big role in sugar spikes.
Good yoga poses include:
- Cat–Cow
- Bridge pose
- Child’s pose
- Surya Namaskar (Sun Salutation)
Slow breathing for 5–7 minutes daily can reduce cortisol levels — which often contributes to Type 2 Diabetes.
Post-Meal Exercise Routine
Even gentle movement after eating is incredibly powerful.
You can:
- Walk
- Stretch
- Climb stairs
- Do light household chores
Aim for 10 minutes — it helps the body manage glucose without allowing large spikes.
Home Remedies and Lifestyle Tips
Small daily habits can support your health journey — especially if you’re trying to prevent or manage symptoms.
Sleep Routine
Quality sleep is deeply connected to blood sugar levels.
Tips for better sleep:
- Sleep 7–8 hours daily
- Avoid screens 1 hour before bed
- Keep the room dark and cool
- Create a calming bedtime routine
Poor sleep can trigger cravings and increase insulin resistance — so rest matters.
Hydration
Water helps your kidneys flush out extra sugar.
Simple rule:
- Aim for 6–8 glasses daily, or more if you’re active.
Avoid sugary drinks or flavored beverages with artificial ingredients.
Stress Management
Stress hormones like cortisol can raise blood sugar — even without food.
Try:
- Meditation
- Journaling
- Deep breathing
- Spending time outdoors
Even 5 minutes of calming practices can make a noticeable difference.
Herbal Support & Supplements (Optional)
Some natural options may help support healthy blood sugar, but they should not replace medical treatment.
Common herbal supports include:
- Cinnamon
- Fenugreek seeds
- Aloe vera juice
- Berberine supplements
Always check with a doctor before starting anything new.
When Should You See a Doctor?
If lifestyle changes don’t help and symptoms continue — or if you have multiple Early Signs of Type 2 Diabetes, it’s important to speak with a healthcare professional.
You should seek advice if you notice:
- Frequent urination
- Constant thirst
- Blurred vision
- Unexplained fatigue
- Tingling in hands or feet
- Sudden weight loss or gain
Early support can prevent long-term complications — and sometimes even stop progression.
FAQs
Q1: What are the first warning signs of Type 2 diabetes?
Some early signs include frequent thirst, increased urination, fatigue, blurred vision, and unexplained weight changes.
Q2: Can early signs of Type 2 Diabetes be reversed naturally?
Yes — for some people, lifestyle changes such as diet, movement, and weight control may help manage or reverse early symptoms.
Q3: Is diet change enough to control Type 2 Diabetes?
Diet is extremely important, but exercise, stress management, sleep, and medical guidance also play a key role.
Q4: How long do early symptoms last?
Symptoms vary from person to person. Some may experience them for weeks or months before diagnosis. The earlier action is taken, the better.
Q5: Do early signs always mean diabetes?
Not always — but if symptoms appear persistently, testing is recommended to confirm whether blood sugar is elevated.
Q6: Can exercise help reduce early signs of Type 2 Diabetes?
Yes — exercise improves insulin sensitivity and helps your body use glucose more effectively. Even simple routines like walking after meals or strength training 2–3 times a week can support better blood sugar control.
Q7: Can Type 2 Diabetes develop without symptoms?
Yes. Some people experience very mild or almost invisible symptoms in the beginning. That’s why routine blood sugar check-ups are important, especially if you have risk factors like family history, obesity, or PCOS.
Q8: Are early signs of Type 2 Diabetes permanent?
Not always. If detected early and managed through diet, movement, weight control, stress reduction, and medical guidance, many early symptoms can improve — and in some cases, even be reversed naturally.
Q9: What foods trigger early signs of Type 2 Diabetes?
Highly processed foods, sugary drinks, refined carbs (like white bread, pasta, sweets), and fast foods can worsen symptoms and cause spikes in blood sugar. Choosing whole grains, proteins, and fiber-rich meals helps improve balance.
Q10: How often should someone get tested if they notice symptoms?
If you notice persistent symptoms, it’s recommended to get tested immediately. After that, follow-up testing every 3–6 months is usually recommended — depending on your doctor’s advice and blood sugar trends.
✔ More symptom-related questions? Read: Diabetes Symptoms FAQs
Disclaimer:
The information shared here is intended solely for general awareness and educational purposes. It should not be considered a substitute for professional medical advice, diagnosis, or treatment. While this content may refer to general health guidelines from trusted organizations, it may not be suitable for your specific health needs. Please consult a licensed healthcare professional before making decisions related to medication, supplements, diet, or diabetes care.
References used for general knowledge include:
- World Health Organization (WHO)
- Centers for Disease Control and Prevention (CDC)
- American Diabetes Association (ADA)
Everyone’s health journey is unique, and results may vary. By accessing or using this information, you acknowledge that the creator or publisher is not responsible for any outcomes or decisions made based on this content.
3 thoughts on “Early Signs of Type 2 Diabetes (Complete Guide)”